Sciatica neuralgia is a complicated diagnosis for patients who endure particular types of nerve tissue malfunction. Neuralgia is defined as nerve pain not due to nociceptor activity. This means that there are no anatomical reasons for pain receptors to fire in the nerve, but they are doing so nevertheless. Most doctors use the term neuralgia to denote any type of neurological discomfort. However, there are cases where the diagnosis is more appropriate than in others. In order to fully understand a diagnosis you have received, be sure to have your doctor explain the conclusion in detail and always ask them any questions you may have.
This discussion explores the neuralgia diagnosis as it applies to sciatic nerve symptoms.
Sciatic Nerve Pain Explained
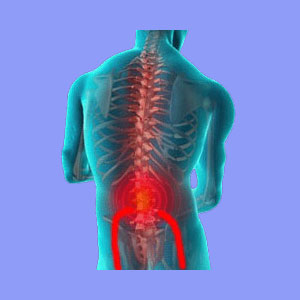
Sciatic nerve neuralgia can affect the actual ischiatic nerve or any of its peripheral branches in the lower body. Sciatica is by far the most common form of neuralgia and can be sourced by a wide range of possible spinal causes. Pseudo-sciatica can also be created by nonspinal and even completely nonstructural causes, as well. These are less often considered compared to the most prevalent diagnostic scapegoats in the lower vertebral column.
In addition to pain receptor malfunction, the patients may also endure a variety of other neurological signal malfunctions which can be responsible for the other common symptoms of sciatica, including tingling, numbness, weakness and complete or partial loss of motor functionality.
Sciatica Neuralgia Diagnosis
All neuralgias are known for being extremely difficult to correctly diagnose. Even the world’s best neurologists often say that their job is akin to educated guess work and some have likened diagnostic methods to the seemingly endless process of elimination, hopefully eventually arriving at a conclusion.
In the majority of chronic sciatic nerve neuralgias I see, the cause is elusive. The treating physician is often far to focused on the Cartesian medical philosophy, which states that all anatomical symptoms have a purely structural source. This forces the diagnostician to thoroughly examine the spine for any irregularity and then blame the pain on the abnormal structural issues, despite times when symptoms do not correlate. This is an epidemic occurrence in the back and neck pain treatment sector.
In many of these cases, the process behind the nerve signal irregularity is completely nonstructural. There will be no anatomical evidence in the spine.
One of the more logical explanations is oxygen deprivation, which is sometimes ascertained by the physician, although the underlying source may be a mindbody process, which usually eludes all suspicion.
Sciatica Neuralgia Conclusions
Neuralgia is a highly unspecific term. When I hear it, I often translate the doctor’s meaning to be: “We know that there is something wrong with this peripheral or central nerve structure. We just have no idea what that problem is or what is causing it”.
In my own pain experience, I have been told by a number of good neurologists that they had no idea what was causing some of my symptoms. This was at least an honest and refreshing change from the scapegoat blame put on a variety of structural spinal issues I have demonstrated for many years. There are strong suspicions that some of my spinal abnormalities are causative or contributory, but there is little definitive evidence of which are the most to blame. I just have so many spinal concerns at this stage of life.
If you have been diagnosed with neuralgia, then you probably know that there is little medical science can do for you, except provide drugs and more drugs. Therefore, it may be worth investigating knowledge therapy as an alternative approach to care.
If a nonstructural mindbody process does turn out to be the true source of your nerve pain, then this treatment may help provide lasting relief. If not, then you have lost nothing and have gained greater insight into the nature of mindbody health. This is a benefit for all, even those who still have pain.





