Sudden sciatica can strike at any time and may be related to a variety of structural, disease-related and mindbody trigger mechanisms. It is crucial that all patients learn what causes sudden attacks of sciatica and how they should be managed until the pain abates. This knowledge greatly reduces the stress level of acute sciatica episodes.
Sudden pain can be very frightening. It can also be debilitating and force patients to miss work, renege on family responsibilities and fear for their future. Sciatica flare-ups are known to be both miserable from a physical perspective, as well as traumatic from a psychoemotional point of view.
This essay helps patients to better understand why and how sciatica can present so suddenly. We will also investigate the best course of action when sciatica does flare up so that patients can be prepared and not be overly concerned with acute symptomology.
Sudden Sciatica Presentation
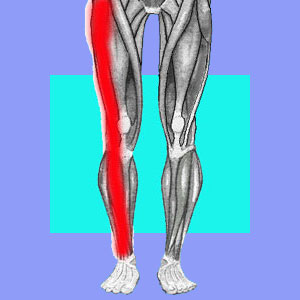
Sciatica can appear on a moment’s notice, with or without warning or a known trigger. Typically, acute presentations will involve severe pain in the buttocks and leg unilaterally, although bilateral variants are also possible. The patient might experience thigh, calf or foot cramps, all of which are commonplace during severe flare-ups of symptoms.
It is typical for numbness and weakness to exist in affected areas of the buttocks and leg to some degree. Tingling might precede pain or continue after acute pain abates.
In very rare circumstances, other symptoms might also exist, such incontinence, objective saddle anesthesia or the inability to stand or ambulate. In these cases, there might be a more sinister reason for symptoms to exist and these circumstances should always be evaluated immediately by a qualified medical professional.
Fast Onset Sciatica Causes
Acute sciatica can be caused by injury, but is also commonly misattributed to perceived injury. When traumatic sciatica exists, it may be due to true spinal sources, such as acute nerve root compression in the lower back, or may be a pseudo-sciatica presentation involving damage to the sacroiliac joint or more commonly, the piriformis muscle.
Sudden sciatica can also occur due to progressive vertebral degeneration that reaches critical mass and causes nerve conduction problems in the spine.
Sciatica attacks can be the result of neuromuscular disease. Many people suffer flare-ups due to diabetes. In fact, diabetes is the fastest growing proven source of sciatica symptomology.
The most common explanation for sudden attacks of sciatica is certainly the mindbody processes. Since psychological sensitivity is a problem that must be managed continuously by the subconscious mind, it is very commonplace for acute symptoms to become necessary at times when repressed and suppressed emotional issues strive for conscious recognition. Since these issues want to escape their confinement constantly, many patients suffer long-term chronic patterns of acute sciatica episodes over many, many year’s time.
First Aid for Sudden Sciatica
When sciatica comes on with sudden fury, it might be best to just relax and try to not stress the body or mind about the pain. Statistics actually support the idea that patients who do not seek treatment and do nothing special for recurrent pain actually heal much faster and better than those who do. This is a very telling fact about the true mindbody nature of pain, as well as the ineffectiveness of most treatments for most conditions.
We generally recommend accepting that the pain exists and using holistic and natural methods of pain management, including heat, ice, massage, acupuncture, mild exercise, stretching, chiropractic and mindbody practices like knowledge therapy and meditation. If absolutely needed, it is ok to take some OTC drugs, but be warned that these products are generally quite toxic to general health. Prescription strength drugs are exponentially worse… Staying motionless in bed is a common practice, but is largely unproductive and causes negative effects on overall wellness, as well as deterring healing of acute pain in virtually all patient profiles.
For patients with recurring symptoms that defy all attempts at treatment, the idea of misdiagnosis should be considered carefully. Most persistent sciatica is misdiagnosed, which is why it has become chronic. Instead of assuming you require surgery for some structural “problem”, it is far more enlightened to take a close look at the validity of the diagnosis and go from there. Once the true source of severe sciatica can be confirmed, curing it becomes much, much easier.





