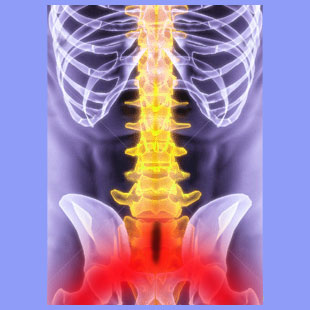
Spina bifida sciatica describes pain, paresthesia or weakness in the buttocks and legs that may be related to a congenital hole in the surface of the vertebral column. Spina bifida comes in 3 classifications and may demonstrate great variation in symptomatic expression.
Spinal bifida occurs in the very first month of fetal development and sets the stage for a lifetime of structural abnormality in the vertebral column. Affected people demonstrate holes in the posterior (and/or occasionally the anterior) surface of some of the vertebral bones. In the worst cases, the actual spinal neurological tissues may protrude from the vertebral canal, potentially causing many serious symptoms. Spinal bifida can be classified as occulta, meningocele or myelomeningocele, each diagnosis offering progressively worse varieties of the condition. Many people who are diagnosed with various manifestations of bifida also demonstrate tethered spinal cord syndrome and other significant backbone irregularities.
This essay examines the incidence of sciatica in people affected by the most common variety of vertebral hole formation: spinal bifida occulta. We will examine traditional medical attitudes towards spina bifida sciatica conditions and shed some objective light on the diagnosis.
Spina Bifida Causing Sciatica
For decades, doctors have blamed even the most conservative cases of spina bifida occulta for being the exclusive cause of pain in any patient who demonstrates vertebral holes in the presence of sciatica symptoms. Treatment was often rendered, but the pain rarely resolved or even improved, despite some drastic and often surgical interventions being employed. The theory here stated that the anatomical irregularity must be responsible for somehow affecting the nerves in the lower back, thereby creating the sciatica syndrome. Strangely, nerve testing was rarely performed in these patients, but if it had been, the glaring error of most of these diagnoses would probably have been obvious.
Mild cases of bifida occulta have long since been almost universally proven to be asymptomatic and not any cause for concern. Of course, since back pain and sciatica are epidemic problems in people without bifida occulta, it was no surprise to see spina bifida patients who also had pain, even though the symptoms were incidental to their irregular spinal formations. There has rarely been any logical process evidenced that could directly cause sciatica in most occulta patients. However, since bifida occulta also increases the chances of being affected with other potentially pathological spinal issues, the sciatica might still be structural, but is simply not a direct consequence of the bifida itself.
Of course, the worse the spina bifida is, the greater the chances of the patient suffering some type of structural pain from the syndrome. Meningocele diagnosis involves a greater risk for pain than occulta, while myelomeningocele patients virtually always have very serious health ramifications to cope with.
The Mindbody Relationship
We already know that many cases of chronic sciatica originate in the mind and are expressed in the body. These pain syndromes are not imaginary or exaggerated, but instead serve a primary gain function to camouflage repressed emotions that remain locked away in the subconscious.
Spina bifida sciatica is certainly not alone in this regard, as virtually any type of chronic pain can serve the same function, from back pain to TMJ to carpal tunnel to fibromyalgia. There is always a link between enduring pain and the mind. In some cases, this link identifies the actual causative process as being psychogenic, rather than purely anatomical.
However, in spina bifida patients, there exists the strong possibility of being affected by the nocebo effect of positive diagnosis. Doctors have blamed bifida as being inherently painful for generations, so it is no wonder that many patients, even now, will believe this mistaken concept subconsciously and allow the condition to actually cause them pain. In these instances, the spina bifida is truly the direct and true source of sciatica, but not for any organic or structural reason. Instead, it is simply the psychological consequence of the diagnosis that creates the pain, once the mind realizes the opportunity for a convincing display of symptoms.
This fact has been proven in countless clinical examples of patients who received diagnostic imaging for a completely unrelated reason and were subsequently told that along with any other findings relevant to the test, that they also demonstrated spina bifida. Many of these people subsequently developed back pain and sciatica, even though they had the bifida for decades, since birth, and had no previous history of pain until the bifida diagnosis was made. This would be impossible to justify on structural grounds alone, but perfectly fits the psychogenic model of symptomology that we know to be such an epidemic concern in the chronic pain treatment sector.
Spina Bifida Sciatica Research
It is well accepted in enlightened medical communities that virtually all cases of mild or moderate bifida occulta are asymptomatic, unless another pathological process exists concurrently. Therefore, patients should never assume that their bifida condition is adequately explanatory for sciatica or lower back pain.
It is vital that bifida patients educate themselves with the latest information, research and statistics available to combat the potential effects of the nocebo phenomenon. Likewise, they must choose their care providers cautiously to avoid being victimized by opportunistic doctors, chiropractors and therapists who sense an easy sale simply by playing up what truly amounts to be a structural nonissue in almost every case.
To learn more about spina bifida, search for our complete site resource section that provides a detailed account of all varieties and effects. To get an objective opinion on whether or not spina bifida is part of the reason for your sciatica pain, talk to your doctor, but be sure to watch for any medical marketing tactics during their evaluation. Just because treatment is not needed does not mean that it will not be offered or even virtually forced on you. Remember that the vast majority of all back, neck and sciatica care provided is not needed, effective or even indicated.





