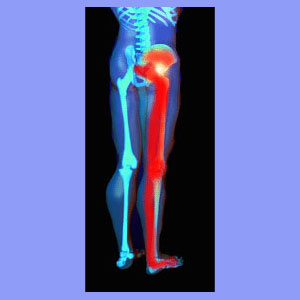
Unilateral sciatica is the most common type of sciatic nerve pain and also the most logical expression of most causative spinal sources. Unilateral means that the symptoms are only present on one side of the body. In the case of sciatica, there are many reasons why a patient might demonstrate pain in only one leg, as opposed to both.
It is crucial to understand that there are bilateral branches of the sciatic nerve, with each leg having its own nerve structure. Additionally, there are 5 sets of nerve roots which make up the sciatic branch on each side of the body. Since structural pathologies are rarely perfectly symmetrical in the spine, many causative processes will therefore only elicit pain on one side, leading to unilateral symptoms.
This article will better explain why patients may only suffer sciatica in the right leg or the left. We will also look at the most common causes of these unilateral sciatica expressions.
Sciatica in One Leg Only
Like all sciatic nerve conditions, there are many potential causes for pain, tingling, numbness and weakness in one leg. Some of the most common diagnoses explaining a unilateral symptomology include:
Asymmetrical spinal stenosis may only affect nerve tracts on one side of the spinal cord or the nerves on only one side of the cauda equina.
Herniated discs generally have a greater chance of causing foraminal stenosis on one side, but not the other. Rarely are both spinal nerve roots affected at the same level, although this is possible with large herniations.
Osteoarthritis will usually cause an osteophyte-induced pinched nerve unilaterally, although severe bone spur or arthritic debris buildup can also enact bilateral symptoms in rarer cases.
Piriformis syndrome can enact unilateral symptoms when only one side of the piriformis muscle is theorized to clamp down on the sciatic nerve.
Sacroiliac joint dysfunction can create sciatica-like pain in some patients and is usually demonstrated on one side only due to joint deterioration or injury, as well as the potential for soft tissue pathologies surrounding the SI joint.
Ruptured discs can cause sciatic nerve pain through chemical radiculitis and this process may only affect the nerve roots on one side of the spinal canal.
These are all typical spinal abnormalities on which most sciatica is blamed. However, research has clearly shown that some of these conditions are often misdiagnosed. The majority of minor spinal structural irregularities are coincidental to the pain and the symptoms typically do not even match the clinical forecast of the diagnosis in many cases.
For example, if a herniation is shown to possibly block the neuroforamen on the right side only, but the patient has bilateral symptoms, then this disc issue is extremely unlikely to be involved in causing the expression. There may another structural or nonstructural process causing the symptoms instead. These types of scenarios must always be considered when a diagnosis is being proposed.
Unilateral Sciatica Condition
Sciatica which is very predictable in its symptoms has a better chance of being caused by an actual structural cause. Patients who experience pain in a specific area, the same way each time, better fit the profile for a physically-induced set of symptoms. This is certainly not a rule written in stone, but it generally applies. Additionally, symptoms will usually be expressed in a particular area of the body which is innervated by the affected nerve roots. In order for most diagnoses to be valid, the actual expression must match the clinical expectation. The possible exception to both of these general rules is central spinal stenosis, which is very unpredictable in its effects.
Unilateral sciatica is typically a bit more patterned than bilateral sciatica pain. Patients who have a regular pain pattern can be slightly more confident in a structural diagnosis than patients whose pain changes frequently.
Of all the patients who write to me with questions about chronic sciatica, approximately 85% to 90% have a variable pain syndrome which changes often or even constantly. It is very difficult to buy into the usual diagnosis of a pinched nerve when the symptoms move around so frequently, vary in severity and specific sensations produced, and even occasionally switch legs.
Unilateral Sciatica Summation
It is so crucial to understand that the locations where the symptoms occur, as well as the nature of the symptoms themselves, are intrinsic to the diagnostic process. Your neurologist will ask you many questions about the areas where you have pain and the types of symptoms you have been suffering, as well as for how long.
Answering these questions accurately will help your doctor to make better diagnostic pronouncements and therefore, increase the chances for successful treatment. I can not even begin to tell you all how often the location or expression of the symptoms makes no sense compared to the diagnosis.
Patients write to us all the time and often include their diagnostic reports. So many structural issues implicated as the source of their suffering could never possibly elicit the symptoms demonstrated. In the majority of these cases, the diagnostician is not a neurologist. In almost every case, when an obviously incorrect diagnosis is made, it is announced without the benefit of verified evidence acquired through neurological testing.
Always be sure to demand full evaluation of a unilateral sciatica syndrome and learn all you can about what to expect from the proposed diagnosis. This way, you will have some idea when you are on the right path and when you might have been led astray.