A herniated disc is the most common structural spinal reason cited to explain sciatica pain. The usual clinical explanation of this occurrence theorizes that a lumbar disc is pressing on one or more of the spinal nerve roots. This pinched nerve is what is causing the lasting pain and neurological symptoms plaguing the poor sciatica patient. While this occurrence is certainly possible, it is rarely the actual source of severe or long lasting pain conditions. In reality, the factual symptomology of a real compressed nerve makes a disc herniation extremely unlikely to be the source of chronic sciatica.
This essay discusses how lumbar intervertebral herniations may enact lower body radiculopathy conditions. However, we will also explore other ways in which bulging discs may cause sciatica, as well as the prevalence of misdiagnosis in circumstantial disc abnormalities.
Herniated Disc Explanation
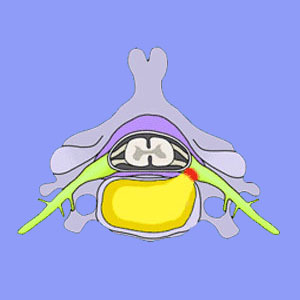
A herniated disc, also called a bulging disc, slipped disc, prolapsed disc or disc protrusion, occurs when the inner core of the disc, named the nucleus pulposus, bulges against a defect in the outer disc wall, termed the annulus fibrosus. The outer wall typically maintains its structure and just bulges asymmetrically. Sometimes, an annular tear develops and the nucleus actually spills out of the disc. This is typically called a ruptured or extruded disc.
Herniated discs are pliable and are not the consistency of bone. It is difficult to imagine them compressing anything, but nevertheless, this is the diagnosis in most suspected pinched nerve events.
The actual process of compressing a spinal nerve root is usually diagnosed as foraminal stenosis, which means the disc pinches the nerve root as it exits the spinal column through the neuroforamen. If the disc instead compresses the entire spinal cord or cauda equina structure, then the condition is diagnosed as spinal stenosis. For a complete encyclopedia of intervertebral disc information, please visit the specialized herniated disc website on The Cure Back Pain Network.
In some instances, a ruptured disc is blamed for spilling theoretically irritating proteins onto sensitive nerve structures, causing radicular pain. This diagnosis is called chemical radiculitis.
Please read more about sciatica from a herniated intervertebral disc.
Also check out why people claim to have a bulging disc pinching the sciatic nerve, even when this is anatomically impossible.
Bulging Disc Causes
Back or neck injury can cause a spontaneous disc herniation. Most traumatic events will cause pain and this discomfort might be severe. However, even the worst of these sudden herniations will usually resolve within 2 to 8 weeks time, with or without medical care. Remember, it is natural for trauma to be painful, even if no neurological tissue is compressed by the herniation.
Normal aging processes, such as degenerative disc disease, can make a spinal disc more likely to suffer a herniation or rupture. However, these degenerative herniations are far less likely to be painful and most go completely unnoticed, since they do not cause any symptoms at all.
Bulging discs are not likely to cause enduring pain, despite their fearsome reputation for doing so. Remember, the basis for most prolapsed disc pain diagnoses counts on the physical compression of a nerve structure. This event may be theorized to be agonizing, but is also scientifically proven not to cause chronic pain symptoms. In fact, research has definitively shown that ongoing compression of a nerve will cause that nerve to stop signaling completely. The resulting effect is numbness, not lasting pain.
Objective View of Herniated Discs
Disc herniations are perhaps the most frightening of all back pain diagnoses. When a patient hears that they have a herniated disc, they are instantly affected by the considerable nocebo effect of the diagnosis. This is a real shame, since most minor herniated discs do not enjoy their fearsome reputation for any tangible reasons inherent to the actual condition. No, the condition is only thought to be so stubborn due to the common misdiagnosis of herniations as the actual source of pain. Of course, herniations will not respond well to any treatment, if they are not causing the pain to begin with. This makes perfect sense.
Remember, herniations themselves are harmless. They can only enact symptoms if they compress or chemically influence surrounding nerve tissue. In most patients, this simply does not occur, although it certainly can and does in a minority of cases.
Learn the facts about sciatica, especially if your pain is being blamed on a lumbar bulging disc. For 18 years, I embraced the diagnosis that 2 lumbar herniations at L4/L5 and L5/S1 were the major cause of my own horrific agony. I tried everything to beat this pain, same as most of you have done. However, nothing worked. These discs do not seem to be anything more than incidental spinal abnormalities, same as most diagnosed disc herniations.
My experience gives me a great segue to my final point. In many patients, lumbar herniations exist, for they are virtually commonplace and the single more prevalent of all spinal irregularities. However, they are not the true cause of pain. Among the many possible other structural and nonstructural causations of sciatica, I want to warn all patients to beware of cervical disc pathologies which enact stenotic changes in the central canal. This cervical spinal stenosis can cause a widespread diversity of symptoms and may not be discovered since the focus of treatment is directed mistakenly at the lumbar region.





