Sciatica caused by surgery is far more common than people think. In fact, many surgical procedures are directly responsible for pain. We receive many letters each month from readers who wonder if various types of surgical interventions could possibly be responsible for creating their sudden bouts of sciatica. Although it seems almost unbelievably naive not to know just how dangerous and damaging surgical endeavors are, we try to provide compassionate answers for each patient. Since we found this topic to be a regular inquiry, we have decided to write a dedicated topical discussion on the subject to help patients understand how surgery might be the root cause of their sciatic nerve symptoms.
This dialog focuses on exploring various surgical techniques and the ways these operations can create sciatica. We will examine spinal and nonspinal surgeries and the reasons why sciatica might begin after the operation ends.
Spinal Sciatica Caused by Surgery
Spinal operations are often very invasive and have the potential to cause all manner of negative health effects. Spinal surgeries are fraught with risk factors and many patients suffer complications during or after their procedures. The more dramatic the operation is, the more these statements hold true. We have been warning surgical consumers of the hazards of various types of spinal surgeries for over a decade and have advocated for changes to the types of techniques used, as well as the indicated uses for these procedures. While some things have changed for the better, there are still many problems with virtually all of the most common invasive spinal treatments.
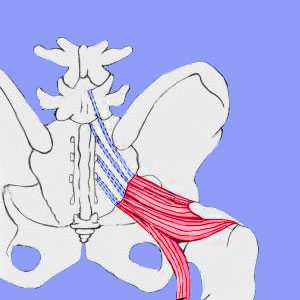
True sciatica comes from compression of the lumbar and sacral nerve roots that form the sciatic nerve. Pseudo-sciatica comes from other spinal sources, non-spinal sources and even non-structural processes that elicit the exact same symptoms as true sciatica. Both of these types of sciatic nerve symptoms can be caused by various types of spinal operations:
IDET, nucleoplasty, discectomy, laminectomy, rhizotomy, kyphoplasty, neurotomy, vertebroplasty and foraminotomy all have the potential to damage nerve roots or even traumatize the spinal cord itself. Nerve damage is one of the major risks of surgical intervention and can be caused directly by iatrogenic error, or may be an eventual result of an unforeseen complication or the subsequent degenerative processes put in motion by the surgery itself.
Spinal fusion, corpectomy and implant placement demonstrate much higher incidences of significant complications and also present more risks to all the tissues of the vertebral column. All of these procedures can damage nerves or the spinal cord, as well as endanger overall health and physical functionality.
Damage may occur to the L4, L5, S1, S2 and/or S3 nerve roots or may occur to the spinal cord tissue tracts that eventually form these nerve roots. Either way, sciatica symptoms are a very common consequence when trauma is caused to any of the spinal neurological tissues that in any way have a role to play in the transmission of motor, sensory or autonomic signals between the brain and the sciatic nerve.
Non-Spinal Sciatica from Surgery
Although spinal-targeting procedures are the worst offenders, other types of surgery certainly also have the potential to create sciatica through many different mechanisms. Below, we list some of the scenarios we have seen that resulted in chronic and often debilitating pseudo-sciatica that was directly created by a non-spinal operation:
The sciatic nerve itself can be damaged by any type of operation that invades the anatomy where the nerve or its peripheral branches traverse. This ranges from the buttocks to the hip to the legs and even the feet. There are countless operations that can be performed in these locations, including tumor or cyst removal, trauma treatment to repair tissue or stop bleeding following injury, repair of a damaged muscle, ligament or tendon in the lower body, internal organ surgeries or pelvic floor procedures in the lower anatomy, hip surgeries and implants, knee surgeries and ankle surgeries.
Damage might occur to the sciatic nerve directly during any of these procedures and may be a collateral consequence of these surgeries and many others. Remember, sciatica can also be caused by anatomical events that might result from these and other surgeries, including infection, disease, muscular imbalances, ischemia (structural, circulatory or mindbody variants all included) or other factors.
We have seen many surgeries causing the piriformis muscle to spasm, enacting sciatica. We have seen many surgeries creating circulatory problems that result in sciatica. We have also seen many cases where the sciatica nerve was directly injured due to surgical intervention, which qualifies as medical negligence in virtually every instance. We have seen a wide range of internal organ procedures create damage that led to the development of diabetes and subsequent arrival of symptoms linked to diabetic neuropathy.
Sciatica Caused by Surgery and Other Treatments
Openly invasive surgery is not the only medical technique that can directly cause sciatica. There are also many other procedures that are found to be responsible for enacting sciatica through the same mechanisms as detailed above. Sciatica caused by surgery or other medical procedure is considered iatrogenic in nature. Some of the most commonly cited of these medical interventions gone awry include:
Epidural injections, discograms, myelograms and other types of diagnostic injections in the spine, hip or sacroiliac joints are all dangerous and can damage the nerve directly through penetrating injury or through chemical irritation.
Arthroscopic hip and knee diagnostic procedures and treatment procedures can affect the sciatica nerve, even when they fall short of being considered actual surgery.
Postoperative Sciatica
Patients must understand that surgery of any type is an injury. The body views surgery in exactly the same way that it does violent trauma of any other variety. Many surgical treatments have the potential to create back pain, neck pain or sciatica, as well as worsen existing pain problems. In fact, most of the surgeries used to treat back pain have the highest risk of actually causing it or worsening it. This explains why so few patients find lasting relief, if any relief, from most forms of spinal operations targeting dorsalgia complaints. Never be naive. If you are facing surgery, make sure to do everything in your power to reduce the chance for complications:
Hire the best surgeon and make them commit to their diagnosis and treatment prognosis. Be sure to research them for their surgical outcomes and check if they have a history of litigation, disciplinary actions or complaints.
Always choose the least invasive type of procedure that can accomplish the surgical goal. Less invasive techniques have less damage potential and usually create fewer complications.
Speak openly with your surgeon about risks involved in the procedure and what can be done to mitigate these factors, such as the use of live x-ray, fiber optics or other live imaging to minimize risks of “blind” procedures.
Most importantly, realize that the vast majority of all spinal surgeries are never necessary to begin with, and the same holds true for a significant percentage of nonspinal surgeries. If the surgery is not objectively necessary, do not undergo it and prevent problems before they occur. It is better to avoid problems than to be stuck with lifelong sciatica caused by surgery.





