Foraminal stenosis is a diagnosis which can be caused by several possible spinal abnormalities, including herniated discs, osteoarthritis, vertebral slippage and atypical spinal curvatures. Some degree of neuroforaminal stenosis is normal to experience as people get older. Most minor to moderate cases are not symptomatic in any way.
However, this does not prevent some asymptomatic stenotic changes from being misdiagnosed as the source of sciatica pain. Stenosis of the foramen encompasses some of the most common and popular reasons used to explain acute and chronic sciatica.
This essay defines and profiles stenotic changes in the lumbar neuroforamen and how these anatomical alterations may be involved in a sciatic nerve expression.
Explanation of Foraminal Stenosis
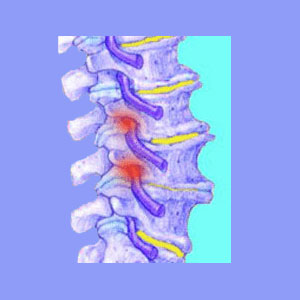
The foramen, also called neuroforamen, are the openings between the individual vertebrae, through which pass the nerve roots as they exit the spinal column. There are left and right nerve roots at every vertebral level branching off either side of the spine. These nerve roots are further broken down into ventral nerve roots, which control motor functions and dorsal nerve roots, which control sensory perception. In essence, there are 4 nerve root components per vertebral level.
The neuroforamen are plenty large enough to accommodate these nerve roots many times over. However, sometimes structural conditions can narrow or block these openings, thereby possibly compressing a nerve root as it leaves the spine. Remember, most cases do not influence the viability of the nerve at all, but when the nerve is constricted, significant symptoms can result.
Causes of Stenosis of the Neuroforamen
There are many possible causes of foraminal stenosis in the lumbar spine, but the following are the most often diagnosed in association with sciatica symptoms:
Herniated discs are the most common diagnosed source of any type of stenosis. In these cases, the disc bulge is thought to block the foraminal opening, causing a pinched nerve.
Osteoarthritis can create bone spurs and arthritic debris buildup around the neuroforamen, limiting the space for the nerve root to successfully exit the spine.
Severe scoliosis, hyperkyphosis or hyperlordosis can all potentially limit the foraminal spaces, especially in the interior apex of irregular curves.
Extreme spondylolisthesis might potentially cause stenosis of the central canal or neuroforamen. When a vertebra moves out of alignment, this will also offset the foraminal openings to a minor or major degree, depending on the diagnosed grade of slippage.
Degenerative disc disease is sometimes blamed as a contributing factor, especially in conjunction with spinal arthritis. As discs dry out, the intervertebral spaces narrow, bringing the bones closer together and subsequently resulting in narrowed foramen.
Foraminal Stenosis Facts
Of all the potential sciatica causes, stenosis of the foramen is the most popular causative theories and is also one of the most often misdiagnosed. Laboratory studies have clearly shown that herniated discs typically do not compress anything and are usually not the source of lasting pain or pinched nerve symptoms.
Studies have also shown that in order for any bone or disc pathology to cause symptomatic stenosis of the neuroforamen, nearly the entire space would need to be closed off by the disc bulge or osteophyte growth, which virtually never occurs.
The very diagnosis of a symptomatic neuroforaminal blockage is often on very shaky grounds, even with severe spinal abnormalities, but the thought that a minor herniated disc or degenerative disc disease causing such widespread and acute sciatic nerve pain is mostly illogical.
Luckily, when it comes to pinched nerves, there should be evidence of nerve compression which can be easily ascertained by any qualified neurologist. Nerve conduction, and other testing, can determine affected nerve tissues and with objective symptomatic correlation, there is really no reason for any patient to ever receive an incorrect diagnosis. Be sure to insist on a thorough neurological evaluation in order to achieve the best diagnostic results for any foraminal stenosis condition.
Pinched Nerves from Stenosis
If you have been diagnosed with a compressed or pinched nerve, due to a herniated disc or osteoarthritic process, be very careful how you proceed with treatment. These are 2 of the most common conditions responsible for leading the patient on a fool’s errand in searching for sciatica relief.
Typically, patients with these diagnosed causes for sciatica do not recover and the simple reason is that the diagnosis is completely incorrect.
My battle with chronic back and leg pain was blamed on DDD and 2 lumbar herniated discs at L4/L5 and L5/S1. These discs were said to be compressing spinal nerve roots, which supposedly explained my pain. Well, I tried everything find sciatica relief, without any success. Furthermore, it became obvious that my symptoms were far too extensive and diversified to be explained by these spinal abnormalities. However, I was the only one who seemed to care about this logic. My medical providers simply hung on to their diagnosis as if it were a life preserver in a frozen sea.
It is no wonder that the more I learned, the sooner I fired each and every one of the doctors who proved their ignorance over time. I have a much better and more enlightened care team now, but I still do not rely on them for any treatment; just monitoring.
In summary, I highly recommend reading all about pinched nerves by using the site search in the right column. There are many informative articles here and these will really help any patient who has not been able to find a cure, despite a positive diagnosis of foraminal stenosis.





