Fractured vertebra sciatica can be caused by acute vertebral break presentations or might be the result of arthritic activity after a fracture heals. Fractured vertebral bones are common in the lumbar spine, making them a primary cause of true spinally-motivated sciatica. However, fractures that occur elsewhere can also influence the spinal cord, potentially enacting sciatica-like expressions even when these injuries occur in the neck (more commonly) or middle back (extremely rarely).
Vertebral fracture can occur for many reasons, including trauma, bone porosity, old age, excessive body weight and other explanations. Not all fractured vertebrae are serious occurrences, but all of these injuries have the potential to enact dire mechanical or neurological effects in worst case scenarios.
This focused essay delves into the creation of sciatica and pseudo-sciatica expressions by fractured vertebral bones. We will detail how fractures can cause sciatica, as well as how they can be treated and resolved.
Fractured Vertebra Sciatica Factsheet
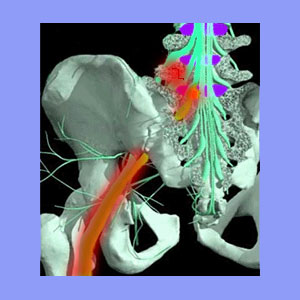
Lumbar fractures can directly compress the lumbar or sacral spinal nerve roots within the central vertebral canal, in the lateral recesses or in the foraminal openings. This can occur with vertebral displacement lacking definitive fracture or virtually any variety of fracture where the broken piece(s) of bone encroach on the neurological tissues. Acute fractures involving great force often migrate and can compress multiple nerve roots in the lower back, potentially creating the ideal circumstances for sciatica to occur.
Occasionally, fractured vertebral bones will completely close off nerve signals, enacting fast-onset objective numbness in the innervated areas of the body. Weakness will follow soon after, although pain may or may not occur. Other less common symptoms of lumbar and sacral nerve root compression may include incontinence, saddle paresthesia, constipation and/or sexual dysfunction.
Cervical spinal fractures can have similar effects on the spinal cord and therefore might produce a very wide range of possible symptoms, including all those listed above, with the additions of the inability to stand or walk, possible neurological symptoms in the arms and potential autonomic consequences on systemic or organ functionality. The spinal cord is a more robust tissue than single spinal nerves, but can still suffer compression, particularly in cases where central cervical stenosis already exists prior to the fracture occurring.
Causes of Sciatica From Spinal Fracture
Fractures in the spine can occur for many possible reasons. In healthy children and younger adults, the cause is virtually always traumatic injury, such as that enacted during motor vehicle collisions, significant falls, sporting injuries or acts of violence. Occasionally, victims might suffer from some type of disease or nutritional deficiency that makes the bones brittle and prone to breaking easily.
In older adults, spinal fractures become far more commonplace. This group of patients can still suffer all the usual traumatic causes of fractures, but are also susceptible to fracture caused by osteoporosis or osteopenia. Additionally, the normal degenerative processes that act on the vertebral bones might dispose some people towards fracture in particular regions of the vertebrae.
Obesity is a major cause of fractures, especially in older patients. Compression fractures might not even make themselves known to the patient with pain, but can sometimes become problematic if they impinge on the spinal or foraminal canals.
Fractured Vertebra Sciatica Treatment
Fractures will usually heal and resolve by themselves, but some may require specialized medical care. Fractures that threaten neurological tissues are usually aggressively treated to prevent permanent nerve injury or paralysis. Open reduction of fractures can be performed alone or in combination with other spinal procedures, such as laminectomy or corpectomy, depending on the circumstances of onset. If the spine is left unstable by injury, disease or surgery, then spinal fusion is often performed to reinforce the vertebral column.
There are specialized, minimally invasive fracture treatments used as well, but these remain controversial for several reasons. The best known of these spinal fracture surgeries include vertebroplasty and kyphoplasty.
Fractures which have long healed can also enact sciatica through the development of severe osteoarthritis and bone spur activity in the scarred region. These accumulations can narrow the central vertebral canal or reduce the patency of the neuroforamen, potentially creating sciatica from the usual processes associated with arthritis. Treatment for these scenarios does nothing to address the fracture, since it is already resolved, but instead focus on relieving the stenotic blockages that are affecting neurological tissues in the central nervous system.





