Pronated foot sciatica describes pain that occurs due to over-pronation of the foot which causes flat-footedness, as well as altered gait and posture. This functional theory of pain is mostly embraced by podiatrists, physiotherapists and some sports medicine specialists, but is doubted by many in the traditional medical arena, especially in cases of mild to moderate severity.
Flat-footedness, also called fallen arches, can be demonstrated unilaterally or bilaterally. The condition is known for potentially causing foot pain issues and ankle concerns in some patients with severe manifestations. However, many healthcare providers doubt that most cases are clinically significant enough to warrant the development of a sciatica pain syndrome, being that the human anatomy is so incredibly adept at compensating for structural irregularity in both form and function.
This essay presents evidence of sciatica that can be linked to over-pronation of one or both feet. We will detail how the mechanism of pronated foot sciatica pain relates to the change of angle of the foot. However, we will also present the counterpoint opinion that many diagnosed cases might consist of nothing but smoke and mirrors and often are revisionary verdicts in a long line of failed diagnostic evaluations.
What is Pronated Foot Sciatica?
Foot pronation describes a flattening of the frontal arch of the foot and turning inwards of the big toe. This condition is the diametric opposite diagnosis as foot supination. Pronated feet appear to roll inward at the ball of the foot, making the knife edge of the foot appear to bend outwards from the ankle joint. In essence, the heel bone is further towards the outside of the body in relative position when compared to the position of the ankle bone. This type of foot abnormality can be demonstrated on one foot only (unilateral expression) or in both feet (bilateral expression) to the same or different degrees. Furthermore, over-pronation ranges greatly in clinical severity from mild to moderate to severe and beyond.
It should be noted immediately that the act of pronation is a normal part of walking and some types of standing. However, over-pronation when the body is standing naturally is the type of flat-footedness discussed in this focused essay.
Feet Pronation Sciatica Mechanisms
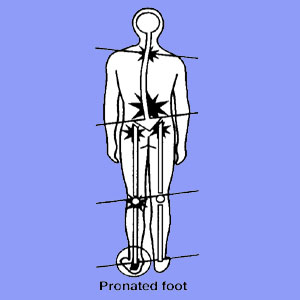
When the feet do not contact the ground as organically designed, the body will have to compensate upwards from the ground all the way to the top of the head. This is the theory used to justify pronated foot sciatica, as well as a plethora of other painful symptoms that may be linked to over-pronation of the foot or feet.
Over-pronation changes the angle that the foot meets the ankle. This might be the end of the effects in some patients, or further compensatory actions might be taken by the body to balance the anatomy due to significant abnormality is posture and gait caused by the foot irregularity. In some patients, the various joints of the knee, hip, sacroiliac and spine will all need to adjust, as will the soft tissues that regulate, ambulate and support these joints. This can create a world of possibilities when it comes to symptomatic expression. For sciatica-specific symptoms, some of the more plausible mechanisms of action include the various consequences of anatomical tilting and compensatory actions:
Postural changes can exacerbate lumbar nerve root compression circumstances, aggravating true spinally-motivated sciatica.
Postural and gait changes can alter the sacroiliac joint between the pelvic ilium and sacrum, potentially contributing to sacroiliac pseudo-sciatica.
Postural and functional all changes can influence the piriformis muscle, causing it to spasm and compress the fully formed sciatic and/or pudendal nerves, eliciting symptoms.
Peripheral branches of the sciatic nerve might be affected by joint or soft tissue changes locally in the upper and/or lower leg. Compression is just one of the mechanisms that might be created by muscular imbalances, joint misalignments and other potential results of over-pronation of the foot.
Some patients suffer multiple internal joint pain syndromes that are mistaken for sciatica. These often affect the hip, knee and ankle, as well as the foot, and exist in combination due to the compensatory actions of the body in response to severe over-pronation.
Pronated Foot Sciatica Doubts
Personally, I was told by a podiatrist that my entire history of back issues was caused by my pronation of the right foot. I found this interesting, since in my case and unbeknownst to this doctor, the pronation condition occurred rather late in life due to a specific injury sustained in martial arts training. My back pain predated it by decades… I did enjoy the opportunity for this doctor to provide a very long and complex explanation for this occurrence, before I set him straight on the facts, much to his chagrin.
Concurrently, we have been researching the opposing viewpoint to over-pronation sciatica for many years already. There are doctors who believe that extreme examples of foot pronation could certainly be the cause of foot pain and possibly ankle pain, as well as some collateral effects higher in the leg and pelvic anatomy. However, these doctors cite that minor to moderate cases of over-pronation (accounting for about 98% of diagnoses) are likely to be nonfactors in sciatica symptoms.
Evidence produced to support these theories includes the human anatomy’s wonderful ability to adjust to changes in “typical” form and function, as well as the proven idea stating that atypical structure is not predicative for pain.
Other doctors state that the explanation of pain being caused by foot pronation is certainly plausible, yet they have personal experience treating patients who demonstrate extreme over-pronation issues, but have never suffered any type of foot, ankle or leg pain, despite obvious postural and gait abnormalities. These doctors make a great case for the idea that over-pronation sciatica is very case-specific and is not universally experienced or expected, nor is it impossible to occur. This supports our findings as well, as we have seen cases where it is plausible and logical based on structural and functional evidence in actual patient profiles, as well as absent in many cases where pain would seem completely justifiable based on severe manifestations of flat-footedness.





