Radiculopathy is another name for spinal nerve root symptoms and is sometimes also diagnosed as radicular pain. The factor which differentiates radicular symptoms from other types of neuralgia is that radicular concerns always involve the spinal nerve roots and are almost always caused by some compressive process within the spinal canal. As with all varieties of nerve-induced pain, there can be a wide range of causes, so an accurate diagnosis is often difficult to achieve. Sciatica is certainly the most common form of lower body radicular pain.
This discussion will define radicular symptoms and explore where and why they occur.
Radiculopathy Expressions
Radicular pain can usually be felt in the area of the back where the nerve compression is occurring, as well as in the areas of the body served by the peripheral branches of that nerve root. Remember, every spinal nerve root has a corresponding anatomical region which it innervates with motor ability and sensory perception.
Sharp pain in the affected area is common and radiating pain, tingling, weakness or numbness in the served area are likely.
Clinical studies of pinched nerves have clearly shown that continued compression of a spinal nerve root will usually cause the nerve to stop signaling altogether. The result of this functional loss is numbness, not pain. Therefore, radicular pain might be severe, but should not continue long-term. Instead, it should transform to tingling, numbness and finally weakness in the innervated region.
Radicular Pain Causes
Radicular pain can be caused by a wide range of potential sources. The sciatica symptoms demonstrated will often provide clues to the vertebral levels which might be affected by compression or chemical irritation. Here are some of the typical causes of radicular symptoms:
Disease processes can damage nerve roots temporarily or permanently.
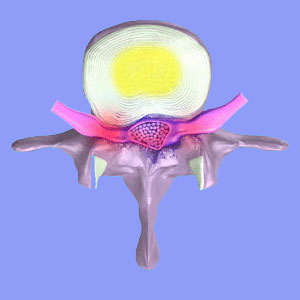
Herniated discs can compress a lumbar nerve root in the central or foraminal canals.
Osteophyte formation can pinch a nerve root or result in arthritic spinal stenosis.
Extreme spondylolisthesis might impinge on one or more spinal nerve roots.
Advanced scoliosis or hyperlordosis might constrict one or more nerve roots.
Most of the above conditions are diagnosed far more often than they actually occur in symptomatic form. In these cases, the diagnosed condition is being used as a sciatica scapegoat to explain otherwise idiopathic symptoms. In these circumstances, there is usually a distinct lack of evidence linking the structural abnormality to the nerve symptoms.
It should be noted that since the spinal nerve roots have already separated off the spinal cord in the lumbar spine, compression can occur in the lateral recess, the foraminal openings or even within the central canal.
Radiculopathy Conclusion
There are so many anatomical possibilities which might create structural lumbar nerve compression, but there are also nonstructural sources of radicular pain, as well. One of the most common reasons for sciatic nerve pain to occur is not structural compression, but rather, simple ischemia of the nerve roots.
Being that this regional process typically exists along with incidental lumbar disc or bone abnormalities, sciatica treatments usually target the anatomical issues, but neglect to do anything to resolve the oxygen deprivation driving the symptom expression. This helps explain why so many patients can not find cures, despite very active therapy regimens.
To summarize this article, the main thought to remember is that radicular symptoms definitively originate in the spinal nerve roots, enacted by compression, chemical irritation or oxygen deprivation. Otherwise, the results are the same as virtually any other true or pseudo-sciatica syndrome. Suffering is the universal factor in all lower back and leg pain conditions, regardless of the diagnosed source.





