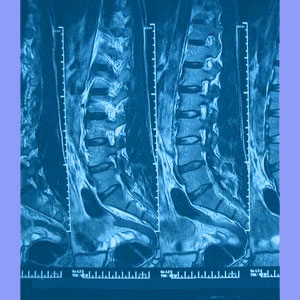
Sciatica from spinal stenosis can be a serious complication of a constricted spinal cord or cauda equina. Spinal stenosis occurs when one or more structural issues narrow the patency of the central canal space. Since this canal contains the central neurological tissues, this can cause spinal cord or nerve compression of epic proportions.
The two most common causes of spinal stenosis include herniated discs and osteoarthritic bone spurs, also known as osteophytes. These conditions will be the focus of this article, but other causes of spinal stenosis leading to sciatic nerve expressions will also be mentioned.
Disc-Related Sciatica from Spinal Stenosis
Herniated discs are the most common of all spinal irregularities. They are so common in fact, that many doctors consider them normal. The mythology surrounding herniations is extensive and gives most patients the idea that all bulging disc conditions are serious and inherently painful. This could not be further from the truth.
Most herniated discs are either completely asymptomatic or only painful for a short time, typically 2 to 8 weeks at the most. Most herniations accused of causing pain through spinal stenosis do not even qualify as true stenosis concerns, since they merely impinge on the thecal sac or abut the cord.
Real purely disc-enacted cord compression syndromes are rare, but can be serious and may require medical or even surgical treatments when they do occur. If the patient demonstrates other contributory factors at the same level, such as ligamentum flavum inflammation or arthritic canal narrowing, then the likelihood for a herniation to produce symptomatic stenosis increases dramatically.
Spinal stenosis can be a serious health crisis. Learn all the facts about the condition from Spinal-Stenosis-Treatment.Org.
Can Vertebral Stenosis Cause Sciatica?
Osteoarthritis is a normal process to experience as we age and it commonly attacks the spinal joints ferociously. Most spinal arthritis is of no significant concern, but sometimes, small bone spurs can grow in groupings, forming what is known as an osteophyte complex. If this occurs inside the spinal canal, the space through which the spinal cord must pass can be sizably reduced, causing a true stenosis condition.
Unlike herniated discs, this type of stenosis is unlikely to resolve on its own and may require surgery in extreme cases. Luckily, most cases of osteophyte induced stenosis are not too serious and usually do not require more than conservative care.
Sciatica from Spinal Stenosis Recommendations
There are other possible causes of central stenosis as well, and all of these may cause or contribute to sciatica in a great number of patients. Spondylolisthesis and various forms of atypical spinal curvature, such as hyperlordosis, hyperkyphosis and scoliosis, may all cause the central canal to lose proper alignment, possibly constricting the spinal cord or cauda equina.
Sciatica due to spinal stenosis is a complicated issue, since the stenosis can affect virtually any part of the spine and still cause symptoms in the lower body. Even spinal stenosis in the cervical spine can cause sciatica in some patients. This makes diagnosis troublesome and treatment less than accurate in most cases.
Remember too that spinal stenosis is incorrectly diagnosed as the actual source of pain in many sufferers. A large sample of the population demonstrates congenitally narrowed canals which are normal for that particular individual and are of no consequence.
Meanwhile, it is also completely normal for the central canal to decrease in size with age and activity, especially in the areas which endure the most degeneration. Just because the central canal is narrowed does not mean anything at all. Only if the spinal cord or cauda equina suffer definitive compression will symptoms occur.
Patients who demonstrate a decreased central canal without verified cord or cauda equina constriction should be very wary of seeking treatment for the theorized canal impingement, since therapy results in these instances are usually very poor.





