Sciatica in certain positions describes symptoms that begin or worsen when the body is oriented in particular poses or postures. Many patients have reported that their pain is positionally-dependent in terms of commencing, as well as escalating or reducing in intensity. However, the interesting thing about positional sciatica is that every patient might have different poses that might help or hamper their pain. There are no common universal postures that make pain worse or better, but there are often similarities in symptomatic exacerbating and relieving positions from patient to patient.
This investigative essay delves into the postural and positional orientations that influence the severity or commencement of sciatica symptoms. We will examine some of these positions and determine why each might have beneficial or detrimental effects on lower back and leg pain syndromes.
Sciatica in Certain Positions / Sitting
Sciatica from sitting is one of the most common of all patient citations. Many patients with lower back troubles discover that sitting is a baneful activity, since it heightens symptoms of pain, stiffness and muscular tension.
Sitting is not inherently bad for the spine and humans have been performing this innocent activity for countless generations. However, when it comes to sciatica, the majority of patients report that continued sitting will exacerbate their symptoms and even enact new ones, such as numbness and tingling in the legs that are not present in other postures.
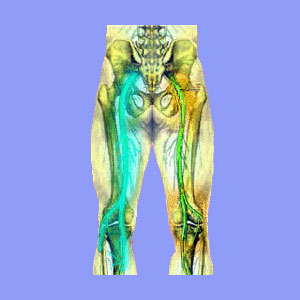
Mechanically, sitting does increase the pressure in the lower regions of the spine, bringing areas of the vertebral bones closer together and possibly reducing the patency of some of the foraminal spaces. Any of these effects might aggravate existing structural issues that are the direct cause of sciatica, including neuroforaminal stenosis.
Likewise, sitting also places stress on some of the soft tissue structures in the lower body anatomy, increasing muscular pressure and possibly enacting direct compression of the fully formed sciatic nerve, often by the piriformis muscle. This piriformis-related pseudo-sciatica is difficult to diagnose and sometimes, is very resistant to many treatment practices.
Sitting also decreases regional blood circulation in the lower back, buttocks and legs, possibly influencing preexisting ischemia conditions that are the underlying causation of sciatica expressions.
It should be noted that some sciatica patients do report relief when sitting, compared to other positions. This might occur due to the body being able to rest or may be positionally-dependent in a positive way, such as in the example of lumbar spinal stenosis patients who enjoy an increase of patency in their particular narrowed central canal levels when the lower back is arched forward.
We find that one of the major contributors to sitting sciatica includes chairs that are too short or too deep for their occupants. Utilizing a straight-backed, shallow chair, that is high enough to allow the knees to point downwards, is almost universally considered the best form of seated posture for lower back and sciatica pain sufferers.
Sciatica When Standing
Standing is also a difficult position for virtually anyone to maintain for extended periods of time. Simply standing in one place increases pressure in the legs, hips, buttocks and lower back tremendously. Some patients might suffer true spinal sciatica escalation when standing, due to body orientation factors. This often occurs in patients with spinal stenosis in the lumbar spine, since standing minimizes the patency of the central canal space. However, many spinal abnormalities might benefit from standing with a straight spine, as opposed to sitting with a sharply curved lumbar region.
Additionally, the muscles of the lower back, buttocks and legs can also contribute to various manifestations of pseudo-sciatica from standing upright. Once again, the piriformis muscle might be the cause of symptoms, especially in patients who stand still and clench their buttocks to provide postural support. This same behavior might also be a prime contributor to the development of hemorrhoids, along with the sciatica symptoms.
Less often considered, but still possible, is the example of patients with severe structural issues in the cervical spine, which respond negatively to a standing posture. Many central cervical spinal stenosis sufferers cite highly escalated lower body symptoms from long periods of standing. These expressions might include numbness, pain and weakness in the legs, as well as possible tightness, burning and pain in the neck and shoulder blades.
A minority of patients, including myself, report pain relief from standing, especially when compared to the terrible torment of sitting.
We advise that if one must stand, it is best to transfer weight back and forth from leg to leg regularly, or to walk about, if possible. Walking typically enacts far less stress than standing still, especially for long periods of time.
Sciatica in Certain Positions / Lying Down
Lying down in a reclined position is usually reported to be the most universally beneficial posture for sciatica sufferers to enjoy. However, even the simple acts of resting and sleeping can become complicated for sciatica victims.
The particular reclining position selected is also a major symptomatic factor for many patients, with some postures being cited as helpful, while others might be considered detrimental, even in the same patient.
The majority of sciatica patients report the fetal position to be the best for providing a pain-free horizontal orientation. This entails lying on one’s side, with the knees bent at a gentle angle. We recommend placing a pillow between the knees and one under the top arm for additional support and comfort.
Patients with unilateral sciatica will often get the best results from the fetal position by placing their painful side up. Patients with bilateral sciatica might or might not see a benefit when lying on the left side, compared to the right.
Some patients find that lying on their back is the most effective for relieving painful expressions in the lower back, buttocks and legs. We recommend that placement of a small pillow in the lumbar arch and another larger pillow under the hollow of the knees will provide improved anatomical support and comfort. Meanwhile, other patients report this supine position to cause increased tingling, numbness and weakness in the low back and legs. I certainly fall into this latter category and try not to end up in this position while sleeping.
Lying prone, face down, is not generally advised. Most people cite that this position causes back and neck strain, even if they do not suffer from any chronic dorsalgia condition. Sciatica patients rarely find this position to be helpful, but in select instances, it may prove useful, particularly when all other positional options fail. If reclining prone is your only option, enhance it by eliminating the use of a pillow all together or using a very thin one.
Suffering Sciatica Pain in Particular Positions
There is no universal answer as to what any given patient must do to find sciatica pain relief. The best one can do is perform trial and error experiments and take note of the results in each position so that they can formulate an effective method of regulating pain based on positional exacerbators and relievers.
One of the best solutions is the idea of constantly changing positions. This plan tells that no single pose is best for sciatica and that any patient can suffer worsened pain by maintaining any posture for too long or under less than ideal circumstances. Instead, patients are told to move about and change positions often. This can be extra work, but seems to provide good outcomes for many patients.
Personally, I can not sit comfortably for long. I stand most of the day, but move about and take lots of breaks to walk, stretch and occasionally sit or lie down for a few moments. While not an ideal solution, this continual revision of anatomical orientation has worked well for me, and for thousands of people who have also adopted the practice.






